WATCHMAN™
Help for patients living with AFib
More than 5 million Americans have atrial fibrillation (AFib), the most common type of heart arrhythmia. One in three patients living with AFib is likely to have a stroke. To reduce this risk, patients may need a blood-thinning medication such as warfarin or other anticoagulant. Some patients who need blood thinners, however, may not be able to take them because of a high risk of bleeding—WATCHMAN™ may be an alternative.
The WATCHMAN™ Left Arial Appendage Closure Device (or, WATCHMAN™) offers select patients with atrial fibrillation an alternative to medication to prevent a potentially life-threatening stroke.
How does the WATCHMAN™ work?
WATCHMAN™ is a permanent implant that offers an alternative to the lifelong use of blood thinners commonly used by patients with Afib. Just like standard stent placement procedures, the device is inserted via a small incision in the upper leg and guided through the artery into the heart.
Once placed, it expands to close off the left atrial appendage (LAA), where blood clots tend to form in people with Afib.
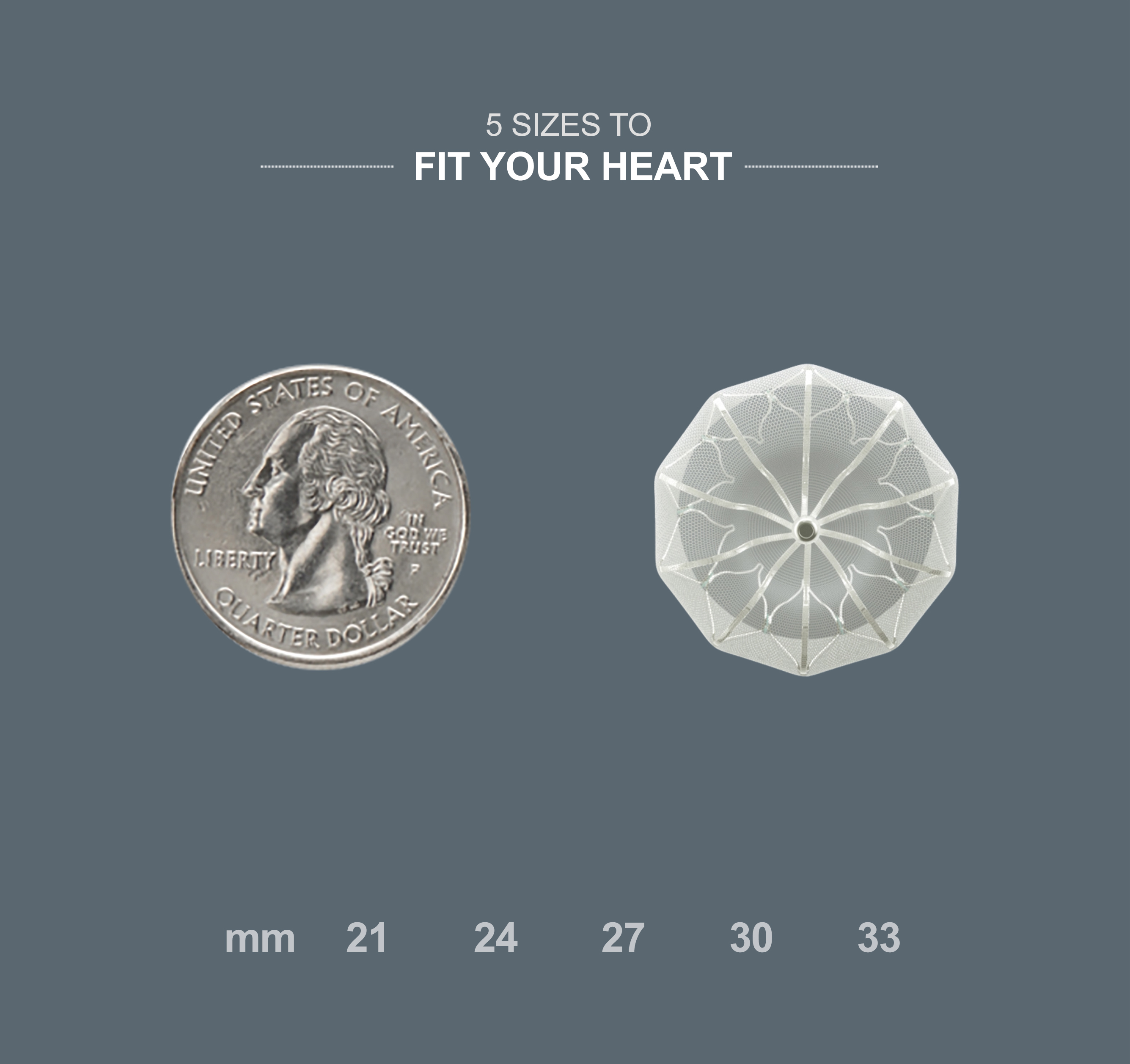
Close to a quarter in size, the device works as the heart's very own 24/7 guard to keep blood clots from escaping into the body.
Who is a candidate for WATCHMAN™?
WATCHMAN™ is approved for patients living with non-valvular atrial fibrillation who have an increased risk of stroke based on CHADS or CHADSVASC scores, are deemed to be suitable for short-term warfarin therapy (45 days) and have a valid reason (such as high bleeding risk or a medication intolerance) to seek a non-pharmacological alternative for their condition.
Frequently asked questions about WATCHMAN™
The WATCHMAN™ procedure is covered for Medicare beneficiaries who meet specific criteria. For a list of the criteria, click here.
The WATCHMAN™ device has been in use internationally since 2009 and was approved by the U.S. Food and Drug Administration in 2015.
This is a permanent implant.
Most medical procedures have risks. Some severe risks include rupture of the LAA during implantation and infection at the site of entry. Ask your doctor to explain all risks to you.
The procedure lasts about an hour.
No, the procedure is conducted under general anesthesia.
The doctor only needs to make a small incision in your upper leg and insert a narrow tube (as done in a standard stent procedure) to complete the implant, keeping wound site and overall recovery minimal.
Most patients stay overnight and are able to return home the next day.
Following your procedure, you will take warfarin for 45 days or until your LAA is permanently closed off. Your doctor will monitor your progress and decide when you are ready to stop taking blood thinners.
Your doctor will tell you what you can and cannot do now that you have the device implanted.