Rotations/Curriculum

Comprehensive, flexible training in family medicine
At Saint Agnes Medical Center, our Family Medicine Residency curriculum is designed to be both comprehensive and flexible, ensuring every resident can tailor their training to align with their future career goals.
Our program has evolved to reflect the current practice patterns of Family Physicians across the country. While many of our graduates pursue careers in outpatient primary care, others choose paths in hospital medicine, urgent care, or advanced training through fellowships in areas such as Sports Medicine, Palliative Medicine, and Geriatrics.
For residents interested in incorporating obstetrics into their future practice, we also provide opportunities to build a strong foundation in women's health and basic obstetric care. No matter which path you choose, our curriculum provides the structure and support to help you develop the skills, confidence and experience needed to excel in any area of Family Medicine.
Track-focused pathways
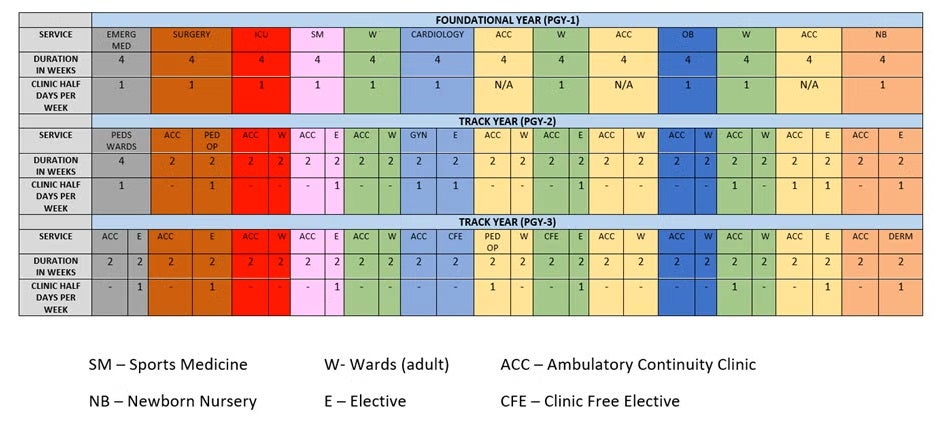
The program has developed a “Track-Focused” curriculum that allows residents to tailor their training towards their eventual career goals. All residents are still required to fulfill the established Family Medicine ACGME requirements with respect to the amounts of rotational and patient care experiences. The Track-Focused curriculum will enable the resident to complete all the necessary requirements in the context of each of their individual career goals through their mandatory elective time. The current ACGME guidelines require that Family Medicine residents have 3 months of elective time, however, proposed changes to these guidelines will expand elective time to 6 months if the ACGME review committee approves in the late Fall.
Starting in the PGY-1 year, residents will rotate through 4-week block rotations that are core to Family Medicine. Every PGY-1 resident will be required to rotate through these rotations. This will provide residents with the foundational knowledge and experience to build upon throughout the rest of their PGY-2 and PGY-3 years.
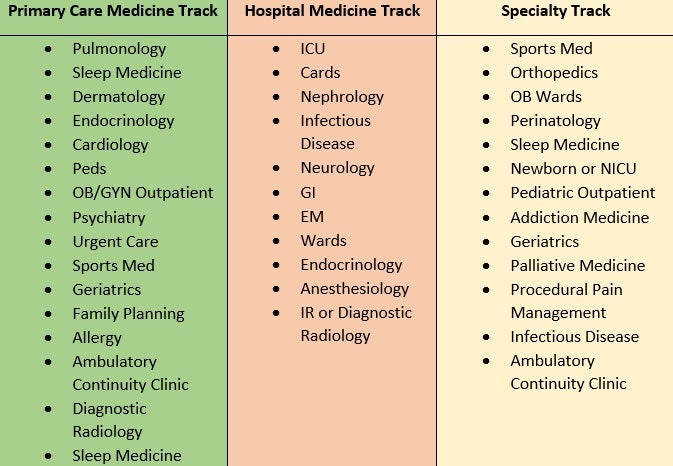
Residents declare a track by the beginning of their PGY-2 year in the following areas:
- Primary Care Focus
- Hospital Medicine Focus
- Specialty Focus (OB, Sports Medicine)
- Global Health Focus
Sample rotation schedule
Residency tracks (elective focus)
Each track contains electives focused on rotations that will prepare residents for their eventual practice goals post residency. The list of electives are not exhaustive. Declaring a track does not in any way commit a graduate to only practicing in that specific track area post-residency. Rather, the track system is designed to optimize graduates' knowledge, experience, and skills toward a particular track. As expected, there is overlap between all four tracks.
Continuity Clinic
Outpatient continuity clinic is a major component of Family Medicine training. In the outpatient continuity clinic, the adherence to specific care requirements is integral to ensuring a comprehensive and balanced approach to medical education and patient care. The composition of resident panels is a key aspect, with a mandate that each panel must encompass a minimum of 10 percent pediatric patients (below 18 years) and a minimum of 10 percent older adult patients (above 65 years). This deliberate inclusion of diverse age groups serves to enhance the residents' exposure to a broad spectrum of medical conditions and healthcare needs. Additionally, there is a commitment to the regular assessment and rebalancing of panel size and composition for each resident. This recalibration, performed every 12 months, takes into account the demographic and medical condition diversity necessary for optimal education, patient access, and the maintenance of continuity of care. By ensuring such standards, the outpatient continuity clinic becomes a dynamic learning environment that caters to the educational needs of residents while simultaneously addressing the varied healthcare requirements of the patient population.
In order to preserve continuity of care, all residents will rotate through their continuity clinic once to twice weekly when assigned to a non-continuity clinic rotation block. If a resident is assigned to be on a continuity clinic rotation for that particular block, they will remain in clinic for four out of five days of the five-day work week.
Inpatient Family Medicine Service
Our inpatient family medicine service is run by our own Family Medicine residents and Family Medicine attendings. We admit general internal medicine patients that come in through the emergency department as well as our clinic patients. The service runs 365 days a year, 24/7 to ensure continuity of care. Every resident is assigned on this service and consists of two PGY-1 level residents and one senior level resident at the PGY-2 and PGY-3 years. Nights are covered by a night float senior resident that is integrated onto the service.
Mobile Health Curriculum
Residents will travel to rural communities around Fresno County to provide basic primary care services. In conjunction with California State University, Fresno’s School of Nursing, residents and faculty will work side by side with members of the Nursing School to assess and care for patients in the community with the aid of point of care diagnostics, a state of the art mobile health trailer, and ancillary staff support.
Learn more about our Mobile Health Unit
Nursing Home Care
All residents are assigned nursing home patients to care for starting during their PGY-2 years. Residents will follow and care for their patients through their PGY-2 and PGY-3 year on a monthly basis. Every effort is made to ensure that residents follow the same patients throughout their last two years of training to maintain continuity. Our family medicine faculty round with residents at their assigned nursing homes within the community.
Obstetrics
Residents will rotate at Saint Agnes Medical Center’s Obstetric Ward. The OB rotation is staffed by the hospital’s OB hospitalist service. Residents will learn the basics of acute OB care. This includes management of obstetrical urgencies/emergencies, NSVD, C-Sections, pre-mature labor, assisted delivery (vacuum delivery), and post-partum care. Our program also cares for low-risk OB patients in our continuity clinics. We also have a Family Medicine faculty who also performs low-risk deliveries with our residents.
Pediatrics/Newborn
Residents rotate through Valley Children’s Hospital (VCH) during their PGY-2 year for 4 weeks for their pediatric inpatient rotation. VCH is the only major pediatric hospital between the Bay Area and Los Angeles and is a major referral center for subspecialty pediatric care. Residents also rotate through VCH’s Emergency Department during their PGY-3 year in order to gain a solid experience in pediatric emergencies. Overall, VCH has a very strong educational experience for our residents due to the broad range of pediatric pathology they encounter.
For community-based outpatient pediatrics, our residents rotate with various community pediatricians who provide our residents with a good foundation of well-child care and sick visits. Additionally, our continuity clinic cares for children of all ages.
Residents are required to rotate on our hospital’s newborn nursery. Aside from expectant care, they will gain experience in diagnosing and treating newborn issues such as hyperbilirubinemia and neonatal sepsis.
Point of Care Ultrasound (POCUS)
Our program features a specialized curriculum for Point of Care Ultrasound (POCUS). Our faculty members undergo comprehensive training through the Global Ultrasound Institute (GUSI) and regularly lead didactic workshops, imparting fundamental POCUS principles to residents and medical students. The integration of POCUS within day-to-day patient care ensures the gradual mastery of POCUS skills over the course of the three-year residency program.
Our POCUS training protocols encompass a range of ultrasound devices, including the GE VScan Air, GE VScan Extend, Butterfly iQ, and a GE standalone ultrasound unit on wheels. This array of devices equips our residents with proficiency in operating different types of ultrasound devices.
The practical application of POCUS is seamlessly integrated across multiple settings. This includes its utilization within our ambulatory continuity clinic, our inpatient service, and our mobile health unit, which extends medical outreach to underserved regions. This versatile incorporation of POCUS further underscores its significance in enhancing our residents knowledge and skills POCUS applications.
Specialty Care Rotations
To ensure our residents are receiving a broad-based educational experience, residents must receive training in various specialties including, but not limited to general surgery, psychiatry, gynecology, sports medicine, and dermatology. Dedicated specialists within and outside of the Saint Agnes Medical Center system provide an in-depth hands-on learning experiences for all of our residents.
Scholarly Activity
Our program requires residents to complete two scholarly projects, which consists of one QI (quality improvement) project and one additional scholarly project such as a case report or original research. With the help of our institutions research coordinator and faculty, residents will have the support they need to complete their projects prior to the end of their training. Our graduate medical education departments hold an annual in-person Research Day in May where all residents from all Saint Agnes Medical Center's GME Residency Programs present and showcase their scholarly activity.
Conferences
Saint Agnes has in person, one half-day per week dedicated time for didactic learning and workshops. The program teaches essential topics encountered in primary care as well as recommended topics from the American Board of Family Medicine (ABFM). In addition, clinic morning reports are routine twice through the week which includes board review and case discussions.
Saint Agnes Medical Center Family Medicine and Internal Medicine are two of the few selected clinical sites in California where residents participate in presenting difficult diabetic cases and receive live teaching didactics from Stanford's renowned endocrinology department.
Board Prep
All residents are provided the following board review materials/activities:
- Uworld Family Medicine Board Review
- ABFM ITE Exam Bank 10+ years
- AAFP Board Review Questions (900+)
- Quarterly MOCK ITE exams
- FP Essentials Subscription
We also purchase each resident their own subscription to a video board review course from National Family Medicine Board Review.